What Is the Best Material to Use for Hip Replacement?
- Review
- Open Access
- Published:
Recent updates for biomaterials used in total hip arthroplasty
Biomaterials Research volume 22, Article number:33 (2018) Cite this commodity
Abstract
Background
Total hip arthroplasty (THA) is probably one of the nearly successful surgical interventions performed in medicine. Through the revolution of hip arthroplasty by principles of low friction arthroplasty was introduced by Sir John Charnley in 1960s. Thereafter, new bearing materials, fixation methods, and new designs has been improved. The master business organisation regarding failure of THA has been the biological response to particulate polyethylene droppings generated past conventional metal on polyethylene begetting surfaces leading to osteolysis and aseptic loosening of the prosthesis. To resolve these issues, the materials of the modern THA were developed since then.
Methods
A literature search strategy was conducted using various search terms in PUBMED. The highest quality articles that met the inclusion criteria and best answered the topics of focus of this review were selected. Fundamental search terms included 'total hip arthroplasty', 'biomaterials', 'stainless steel', 'cobalt-chromium', 'titanium', 'polyethylene', and 'ceramic'.
Results
The initial search retrieved 6921 articles. Thirty-two manufactures were selected and used in the review.
Conclusion
This article introduces biomaterials used in THA and discusses various bearing materials in currentclinical use in THA likewise as the newer biomaterials which may even further decrease wear and improve THA survivorship.
Groundwork
Total hip arthroplasty (THA) is 1 of the most popular surgical procedures performed worldwide. In England, the National Joint Registry recorded that more 790,000 THAs were performed betwixt 2003 and 2015 [1]. As of 2003, more than 200,000 THA operations were performed annually in the Usa, about 2.five million people are living with a hip replacement [2]. This number is expected to attain 572,000 by 2030 [three]. In Korea, the Health Insurance Review and Assessment Service informed that more than than lx,000 THAs were performed betwixt 2010 and 2017, and incidence was increasing over fourth dimension [4].
Current developments in the field of bogus hip joints are focused on mechanical force, biocompatibility [five,6,7,8], bioactivity [nine,10,xi,12,13,14,15,sixteen,17,18] and materials that impart amend wear resistance and mechanical reliability [19,20,21,22,23,24,25,26,27,28]. When an implant fails, patients may endure severe hurting and inability and require revision surgery. Periprosthetic osteolysis is the principal crusade of failure that is the result of activation of an innate immune response caused by wear of bearing materials in THA. Taken up by macrophages and multinucleated giant cells, the presence of wear droppings particles may cause the release of cytokines, thereby resulting in inflammation that further activates osteoclasts and finally leading to implant loosening.
The functional goal of joint arthroplasty is to return a patient to activities of daily living and range of move in the absence of pain. Thus, various biomaterials have been used and are constantly beingness developed. The purpose of this review was to provide an update on the development status of various materials in THA.
History of evolution of Total hip arthroplasty
Metallic on metal (MoM) bearings were made using large ball diameters during 1955–1965 [29]. Even so, the use of MoM bearings declined in the 1970s for some years after Sir John Charnley introduced a THA device based on metallic on polyethylene (MoP) equanimous of a small metal brawl and a cemented polyethylene (PE) cup in a 1960s [thirty]. Long term survival of these early implants was practiced, with around 77–81% of success rate 25 years after main THA [31]. With the increasing employ of THA in younger and more than active patients, the revision rate becomes higher [32], and in that location has been concerns about the role of PE wear particles in osteolysis and loosening [31]. New materials take been introduced to prevent wear and osteolysis.
Pierre Boutin, a French surgeon who anticipated the problem of "polyethylene disease", began using alumina ceramic on ceramic (CoC) hip implants in a 1970s [33]. CoC implants have been used in THA and these developments as well created ceramic on polyethylene (CoP) combinations equally competitive bearing culling along with MoM and CoC over 1963–1973 (Fig. 1).
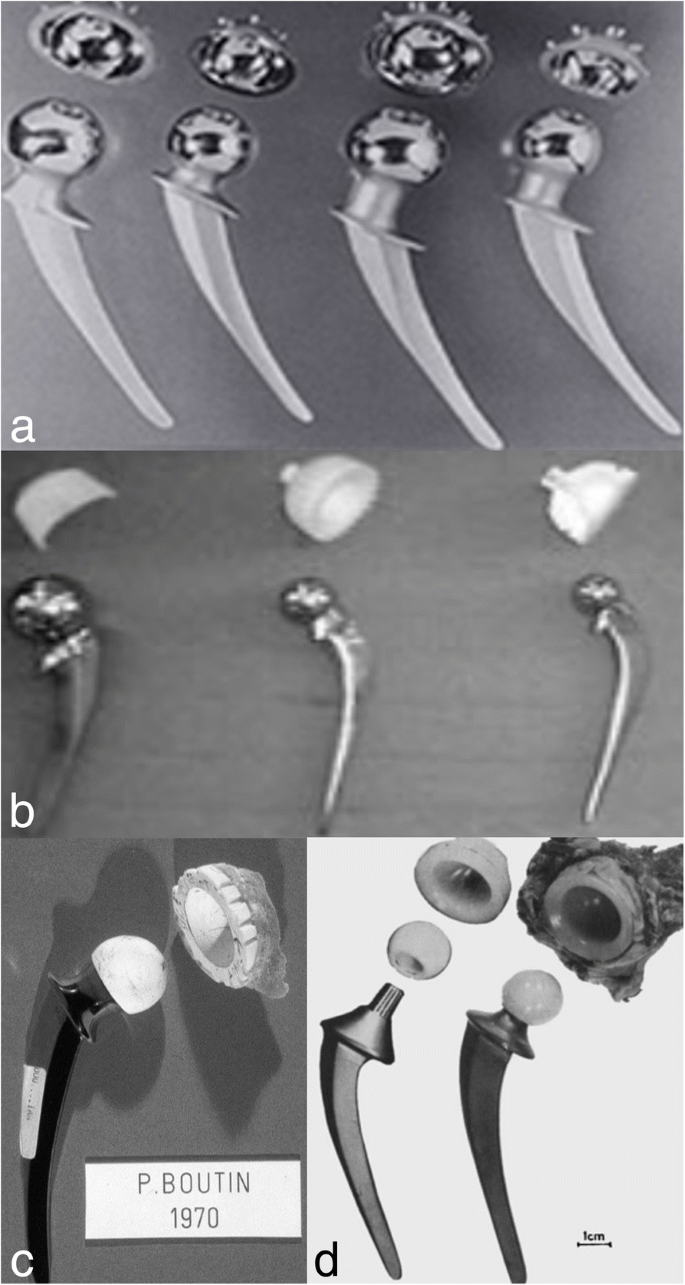
Early on bearing materials used in THA (a) MoM Mckee-Farrer THA from 1960 (b) MoP combinations, Thompson prosthesis in a 1960s (c) CoC hip implants in a 1970s (d) CoP combinations over 1963–1973
Stainless steel was the first class of alloy introduced for orthopedic implants [34]. However, since some corrosion was inevitable, it has been recommended that stainless steel merely be used for brusk duration purposes [35]. Currently, the most frequently used artificial hip joints are equanimous of an acetabular cup, liner, head and stem. The main materials for THAs were titanium, cobalt-chromium, PE, and ceramic, respectively.
Supporting metal materials
Stainless steel
Stainless steels are iron-carbon based alloys. In general, these alloys comprise Cr, Ni, Mo, Mn and C. The austenitic (316 series) alloys are typically used in fracture-fixation devices. The resistance to oxidation coupled with relative ease of machining, forming, and hardening makes stainless steel a strong candidate for material choice. Stainless steel is rarely used for THA textile nowadays, because of poor biocompatibility, though stainless steel devices remain available in other countries (particularly the U.k.).
Cobalt-chromium (co-Cr) alloys
Co-Cr alloys which was used in dentistry, are now one of the major materials used for hip prostheses. The favorable strength, corrosion, and clothing characteristics make alloys of Co-Cr one of the main choice as an implant material. It is mainly used as cement type femoral stem material because the Young'due south modulus is larger than titanium alloys and articulating head due to wear resistance.
Titanium alloys
Titanium and its alloys are pop metal implant biomaterials used in THA. Commercially, α + β titanium alloys, such as titanium-6Al-4 Five have been the most normally used alloys for stem and acetabular cementless components of THA, because of its comparatively low density, high mechanical strength, excellent corrosion resistance, and biocompatibility with bone [36].
However, Titanium alloys are not used for manufacturing of femoral caput due to their poor article of clothing resistance.
During the last ii decades, vanadium free titanium alloys such as α + β titanium-6Al-7Nb alloy with improved biocompatibility have been developed by incorporating biocompatible elements such equally Niobium [v,6,seven,viii]. Many researches have been devoted to the development of bulk metal materials that accept lower Young's modulus, amidst which β titanium alloys have attracted meaning attending.
Alloy surface modifications
Classic implants are fabricated using traditional materials (sintered beads, cobweb metal, plasma spray) which have several inherent biomaterial limitations. In order to achieve an effective osseointegration with a vital bone implant contact and reduce adventure of loosening, the use of porous metals andcoatingswere developed [37]. In general, compared to stainless steels and Co-Cr alloys, titanium, some of its alloys and tantalum are the more suitable porous metallic materials used for orthopaedic applications.
Hydroxyapatite has been used in order to achieve the permanent mechanical fixation of an implant in the os bed to involve the procedure of osseointegration [38]. Porous metal has been likewise introduced to obtain biological fixation and improve longevity of orthopedic implants [39]. The new generation of porous metal has intriguing characteristics that allows bone healing and high osteointegration of the metallic implants [forty].
Materials used in begetting surface
Polyethylene
UltraHigh molecular weight polyethylene (UHMWPE)
UHMWPE was start introduced in 1962 as the begetting for the Charnley hip prosthesis. He adult the low-friction arthroplasty consisting of cemented fixation with a begetting surface of a 22.25-mm metallic femoral head andan all-PE cup [41].
Conventional PE is sterilized by gamma irradiation in air. This process offers the benefits of molecular crosslinking just can also produce gratis radicals that is oxidized in the presence of air [42]. Oxidation decreases resistance of the biomaterial, resulting in degradation and brittle PE, and thus may increase wear [43]. PE wearable is multifactorial: amid the different factors associated with wear are a patient's higher activity level, a large femoral-head diameter or sparse PE liners, vertical orientation of the acetabular loving cup, or the use of modular uncemented cups [44, 45]. UHMWPE wear debris mediated osteolysis is widely recognized as one of the most serious challenges in hip arthroplasty [46, 47].
High crosslinked UHMWPE (XLPE)
The developmentof new XLPE is aimed at improving UHMWPE in both cemented and uncemented implants. In club to subtract PE article of clothing, research has attempted to ameliorate habiliment resistance while maintaining mechanical properties and eliminating the oxidation process [48].
Crosslinking is achieved past using either gamma radiation or electron beam radiation to break the molecular bonds. All manufacturers produce XLPE based on three processes: crosslinking, oestrus handling, and sterilization while avoiding exposure to air. Higher crosslinking density is obtained using gamma irradiation or electron beams at a dose between l and 100 kGy to increase wear resistance. Estrus treatment is aimed at eliminating gratis radicals that appear later crosslinking; this thermal treatment applies temperature in a higher place (remelting) or beneath (annealing) the melting transition temperature of the polymer (137 °C).
In vivo studies, Manning et al. reported 95% wearable charge per unit reduction, and Martell et al. showed 42% to fifty% wear charge per unit reduction using XLPE compared to conventional PE [49, fifty]. Biologic activity of the wear debris was as well reduced and osteolysis has been dramatically decreased [49,50,51,52,53,54].
Antioxidant doped polyethylene
In efforts to amend oxidation resistance without compromising mechanical backdrop through thermal treatments, XLPE is stabilized by the add-on of antioxidants like vitamin East, to prevent oxidation of gratis radicals with the intention of increased wear resistance [xix, 20, 55]. Although initial results are promising, longterm clinical results of this second generation Pes are not yet available.
Poly (2-methacryloyloxyethyl phosphorylcholine) (PMPC)
Kyomoto et al. made a great progress in tribological aspect of XLPE [21]. XLPE has been surface-treated on the articulating surface, covering the surface with a chemically thin layer (100–200 nm) to better chafe resistance. Poly (ii-methacryloyloxyethyl phosphorylcholine) (PMPC), which is formed by photo-induced graft polymerization, creates a super-lubricious layer that mimicks articular cartilage [22]. A recent hip simulator report reported that MPC polymer grafted on the XLPE surface dramatically reduced the article of clothing up to 70 meg cycles [56].
Ceramics
Alumina
Alumina has been used equally a bearing surface in total hips since the 1970s [57]. Alumina ceramics have biocompatibility, high wear resistance, and chemic durability. Habiliment was as low as a few microns for a 15-yr menses in utilise, which is 2000 times less than a regular MoP sliding couple and 100 times less than a MoM prosthesis [58].
Although alumina ceramics have shown better wearable characteristics than MoP, alumina has historically had a high incidence of fracture [59]. This loftier incidence of fracture led to improved manufacturing processes which was possible by decreasing grainsize and porosity, and by tempering process for the increase of toughness [threescore].
With the improvements made in alumina material properties, the incidence of fracture has declined dramatically in recent years. The decreased incidence of fracturing of alumina components has made ceramics a more feasible option, peculiarly for younger, more agile patients [59].
Zirconia
Zirconia femoral heads were introduced in Europe in 1985 and afterwards introduced into the USA in 1989 [61]. The motility from alumina to zirconia as a femoral head component was because of the high incidence of fractures of alumina heads and the increased fracture toughness of zirconia compared to alumina [62]. Zirconia as well had a historically higher bending strength than alumina [63].
However, in view of the recently reported potential for zirconia ceramics to undergo monoclinic stage transformation in vivo, with resultant increased fracture risk and degradation of wear properties [64, 65]. Unfortunately, the largest manufacturer of zirconia femoral heads recalled their products in 2001, because of problems with the thermal processing associated with those batches [61]. Since the recall, use of zirconia stabilized with yttria has declined, only a trend toward developing alumina-zirconia composites to improve performance of ceramic bearings has emerged [66].
Alumina-zirconia composites
Despite the long clinical history of alumina and zirconia in THA, both materials had drawbacks. Attempts to overcome the weaknesses of these materials past combining alumina'southward hardness with zirconia's toughness take led to the development of zirconia-toughened alumina (ZTA), which was commencement commercialized past CeramTec nether the trade name of BIOLOX® Delta in around 2000. ZTA is an alumina matrix blended containing 75% fine grained alumina of 0.5–0.half-dozen μm in bore and 25% Y-TZP with a grain size of 1 μm or smaller to obtain a flexural strength of 1200 MPa and a fracture toughness of 6.v MPa√one thousand [66]. The base alumina matrix ensures high hardness of the materials, and the addition of zirconia particles promotes resistance to crack propagation [62]. ZTA likewise slows downward the kinetics of hydrothermal aging, which is a potential reward over monolithic zirconia.
Silicon nitride
Silicon nitride is a non-oxide ceramic material with high strength and toughness and has been used equally bearings, turbine blades for more than 50 years. In the medical field, since 2008, information technology has been used in cervical spacer and spinal fusion devices, with few adverse reports among 25,000 implanted spinal cages [67, 68]. Silicon Nitride has been recently regarded as a begetting textile for bogus hips due to its high biocompatibility, moderate Vickers hardness of 12–13 GPa, Immature'south modulus of 300 GPa, high fracture toughness of 10–12 MPa√g and flexural force of 1 GPa, with a typical grain size of 0.6 μm afterward alloying with small amounts of yttria and alumina [69]. Mechanical testing has shown higher fracturetoughness, higher flexural force, college resistance to hydrothermal degradation. Biocompatibility tests haveshown that Si3N4 does not produce any adverse reactions behaving similar to alumina [seventy].
Recent hip simulator studies evidence that self-mated silicon nitride couples exhibit up to 3 million cycles of wear compared to self-mated alumina; nevertheless, some self-mated silicon nitride couples bear witness increased vesture at the end of 5 million cycles compared to alumina CoC [71]. Farther long term clinical studies of retrieved heads of silicon nitride and hip simulator studies by others may be necessary.
Hybrid Pattern of Oxide Ceramic Layer on metal (Oxinium™)
A new zirconium alloy (Zr-ii.5Nb) was introduced to hip arthroplasty in 2003 [68]. When heated in an air environment, the surface of the metallic zirconium converts to a black zirconium oxide which is approximately 4 to 5 μm thick [sixty, 72, 73]. This oxidized zirconium femoral head commercialized equally Oxinium™ (OxZr; Smith & Nephew, Memphis, TN, United states of america) is non a coating, but a surface transformation by oxygen improvidence hardening process, which is expected to provide improved resistance under load begetting. It is a relatively new material used as an culling to alumina or zirconia ceramics, demonstrating increased hardness and decreased surface roughness like to zirconia, but possessing inherently high fracture toughness and fatigue forcefulness considering of the metal substrate [74].
In a simulator study, it was observed that Oxinium™ heads produced 45% less wear than did shine Co-Cr heads, and, when the heads were roughened, the difference was much greater, with oxinium producing 61% less clothing. Lewis et al. compared l Co-Cr and 50 oxinium heads and observed the clinical outcome to be equivalent at ii years of follow-upwards [75].
Despite the clinical employ of OxZr's caput for more than than 8 years, nosotros need more reliable data about long term outcomes.
Ultra-difficult coatings on metals
While Co-Cr alloy in cocky-mated configuration or the blend heads sliding against PE or XLPE are frequently used in THA, over l% of failed artificial hipjoints are mainly due to osteolysis mediated hygienic loosening in addition to metal ion allergies overa long term period [76]. A frequent used alternative hybrid approach is to glaze metal alloys with very hard, biocompatible surface layers such equally diamond-like carbon (DLC, 5000 HV) [77] or titanium nitride (TiN 2100 HV) [78].
This approach ensures that the original properties of high strength metallic substrate are retained while: (a) supporting a bearing surface; and (b) avoiding the release of toxic metallic ions from the underlying the Ti alloy substrate. Still, there are several problems such as local delamination, crack corrosion, third body wearable [78, 79]. Some other method is to deposit pure diamond on the metal head. In this regard, coating of ultra nanocrystalline diamond (UND) with grain size of 3–100 nm was directly applied to Ti and Co-Cr blend using microwave plasma CVD [fourscore, 81]. UND coatings possess high hardness (56–lxxx GPa) and depression surface roughness, high wear resistance to third-trunk wear particles [82]. Still, big compressive stresses are retained in the UND blanket due to impurities at the grain boundaries, affecting the adhesion to the substrate [83]. In short, farther enhancements to these blanket techniques are needed to meet the high wear resistance, mechanical reliability and adhesive requirements for prolonged THA.
Clinical aspects of bearing surface
Bearing couples should accept a low coefficient of friction, high surface hardness with lowductility and scratch resistance, and generate a depression volume of wear particles. Moreover, surfaces exposed to tissues should be non-cytotoxic, biocompatible, and bioinert [84]. There are several begetting materials that are commonly used in clinical practice (Fig. ii).
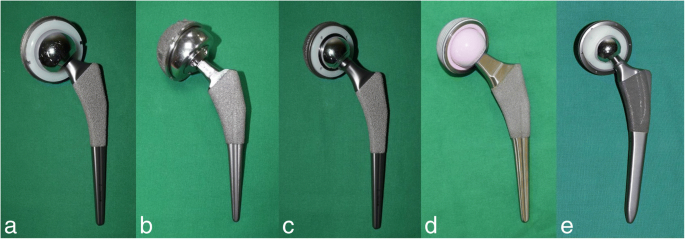
Recent bearing materials used in THA (a) MoP bearing (b) Large head MoM bearing (c) Small caput MoM begetting (d) CoC articulation (east) CoP joint
MoP articulation
Advantages
MoP equanimous of a small metal ball and a cemented PE cup in 1963 [85]. Over the concluding few decades, i of the nigh acceptable begetting surface couple in a prosthetic hip is a Co-Cr femoral head articulating with a UHMWPE acetabular component in view of the excellent Long term results available. Tsukamoto M et al. reported that XLPE grouping presented a significantly reduced wear charge per unit compared with the conventional PE group (XLPE groups, 0.035 mm/yr.; conventional PE grouping, 0.118 mm/yr) [86]. This bearing surface couple remains the i of the standards to which habiliment testing for other begetting articulations are compared. MoP bearing surface, a bearing surface with good long term results in elderly patients, once was taken as gold standard for THA [87].
Disadvantages
It became articulate that PE liner article of clothing droppings generated with time was associated with the occurrence of osteolysis which leads to subsequent loosening and eventual implant failure (Fig. 3). This osteolysis appears tooccur more than commonly at wear rates of more 0.1 mm/yr. and is uncommon when article of clothing rate is less than 0.05 mm/year. [88, 89]. Information technology has been reported that the osteolysis charge per unit of MoP is as high as 26%, and hygienic loosening charge per unit is three% at 10-twelvemonth follow up [ninety].
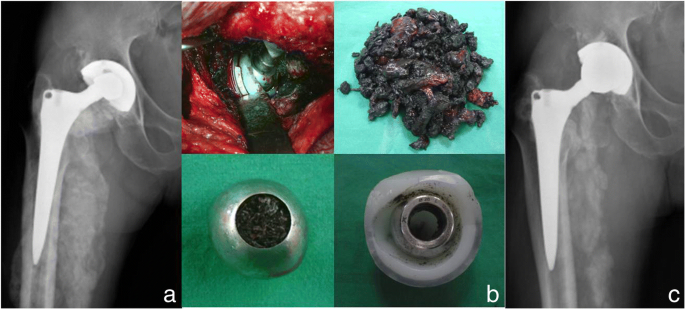
A 62-twelvemonth-one-time male person patient with right full hip arthroplasty using MoP bearing (a) Radiograph illustrating liner wear and metalosis (b) Astringent metalosis and osteolysis (c) Radiographs afterwards revision surgery including excising mass, changing to metasul liner and metal caput after cementing
During the past decade, dissimilar manufacturers have begun to develop new biomaterials in order to decrease PE vesture, such as XLPE, Antioxidant Doped Polyethylene and PMPC. Brach et al. reported better functioning past this newer XLPE than with conventional or even kickoff-generation XLPE [91]. The other strategy is to introduce vitamin E, the antioxidant alpha-tocopherol, into UHMWPE prior toconsolidation to assist forestall the oxidative degradative reaction. This would avert the deleterious result of the melting process that decreases the mechanical backdrop of PE. Oral et al. reported adept habiliment and improved mechanical and fatigue backdrop [92]. However, these new technology whose success and bear upon volition be determined in the longer term. Analysis of retrieved components and clinical results will go along to inform usa on the effects of wear problems [93].
Wear machinery
Adhesive features have been constitute on the surface of PE cups matched with a metallic ball [94]. Welding between the cup and ball generates fibrils on the surface of the polymeric textile. These fibrils may become torn off and pulled away as loose particles. Without sufficient lubrication, bigger fragments may be transferred from counterbody to trunk and vice versa. Such particles may introduce chafe in the form of two or three body abrasion resulting in scratches on the surface.
MoM joint
Advantages
Proposed advantages included the reduction in wear, improved range of movement and a lower dislocation rate [95, 96] and MoM bearings have wear rates that are 20 to 100 times lower than metal-on-conventional polyethylene [97]. MoM THA using a 28 mm head has shown favorable results compared with big caput MoM THA. Pocket-sized head MoM showed a relatively low rate of aseptic loosening at a mean follow up of 20 years [98]. Yoon et al. reported that good clinical results with no complicationsin THAs with MoM bearing even with chronic renal failure [99]. Small head MoM bearing seems to have expert results, relatively.
Disadvantages
The issues with large dewdrop MoM began to appear in 2005. With increasing clinical experience, the national joint registries have recently reported the failure charge per unit of THA with MoM bearings to be two–3 fold higher than gimmicky THA with non MoM bearings [100, 101] associated with local bone and softtissue necrosis, with pseudotumor formation comprising a predominantly lymphocytic inflammatory reaction [102, 103] and, vesture particles in the form of cobalt and chromium ions have been detected throughout the body [104]. Although granuloma accept been found in both the liver and spleen [105] and increased chromosomal translocation has been found within lymphocytes [106], in that location is currently no hard evidence that this leads to neoplasia [107].
Furthermore, midterm studies demonstrated increased rates of osteolysis and implant.
Failure (Fig. 4), raising concerns about the longevity and safety of this begetting surface [108,109,110]. Korovessis et al. followed 217 patients who underwent a principal THA using a second-generation, large diameter MoM bearing surface for an average of 77 months [108]. During this follow up period, 14 THAs (6.v%) were revised and found to have concerning signs of metallosis and lymphocytic infiltrates raising concerns almost this bearing surface. Park et al. followed 169 hips who underwent THA using a second-generation MoM bearing surface for a minimum of 24 months and noted 10 hips (5.9%) had early osteolysis [110]. The poor functioning associated with large caput MoM bearing surfaces led the Food and Drug Administration to remove several second-generation MoM THA systems from the marketplace, finer ushering out the era of this bearing surface [111].
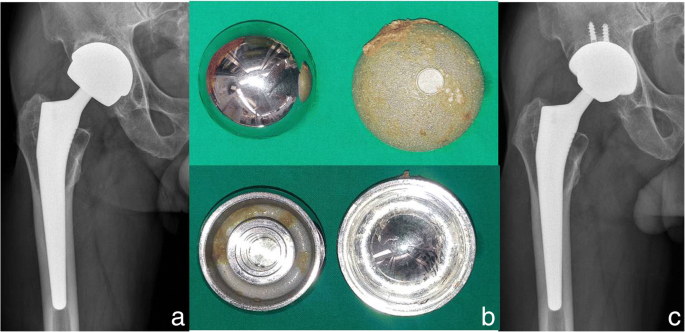
A 68-year-onetime male patient with correct total hip arthroplasty using large head MoM bearing (a) Preoperative radiograph of acetabular aseptic loosening (b) Big head MoM begetting (c) Radiographs afterwards acetabular revision using CoC bearing
Vesture mechanism
The dominant wear machinery is determined to be mild surface fatigue. Surface fatigue is introduced by straight solid contact of surface asperities or by foreign and/or system inherent third bodies, which repeatedly slide or curlicue within the vesture track. Although these third bodies contribute to fatigue related wear loss, this vesture is several orders of magnitude smaller than would exist introduced by adhesion. Tribochemical reactions besides comprise an important wear mechanism in MoM hip joints. They might be triggered by the synergistic interaction of article of clothing and corrosion and tin influence the tribosystem in a positive or negative manner.
CoC articulation
Advantages
In the late 60s, CoC bearings were first introducedin hip arthroplasty by Boutin [112]. They have undergone many generations of changes since so during which the susceptibility to fracture (a problem in early on generation ceramics) has been overcome. Since ceramics are harder than metals, are biologically inert and have meliorate lubrication properties leading to low clothing rates [113], CoC bearings make an attractive option for ensuring long term survival of hip prosthesis. The minimal wear particles released from CoC bearings are also biologically relatively inert and at nanometric size, significantly reducing the osteolysis produced due to PE wear particles. In addition, CoC bearing combination likewise has lesser coefficient of friction, college wettability with biologically inert clothing particles [114]. Clinical results have confirmed college survivorship, lesser wear and depression osteolysis making these bearings an excellent choice for young and active individuals [115]. Yoon et al. reported no instance of osteolysis after 3rdgeneration of CoC bearing THA [116] and lower rate of osteolysis has been confirmed by many other studies [117, 118].
Hernigou et al. investigated wear and osteolysis in bilateral arthroplasties (one CoC and the contralateral CoP) of patients who had survived 20 years without revision and without loosening of either hip [119]. The number of lesions was higher on the side with Cop couple. Hai-bo Si et al. reviewed several manufactures that wear rate was also lower in CoC than CoP THA [120].
CoP articulations also reportedly have reduced wear rates compared to metal heads on PE in THA [121].
Disadvantages
Though the ceramics are the new preferred bearing surface, specially in the young, they are not without their share of complications which include squeaking noises, stripe article of clothing, a rare begetting surface fracture or chipping during insertion. Complications have been more usually associated with acetabular component malposition (more than vertical cups), smaller femoral heads and non-adherence to meticulous surgical technique [122, 123]. Fracture of a ceramic head and/or liner remains a major disadvantage for this bearing combination compared with MoP or MoM (Fig. 5). Earlier generations of alumina ceramic heads had a reported gamble for fracture until 13.4%, however for newer implants (Biolox Forte and Delta) the reported fracture rate is much lower at 0 to iii.two% [124, 125].
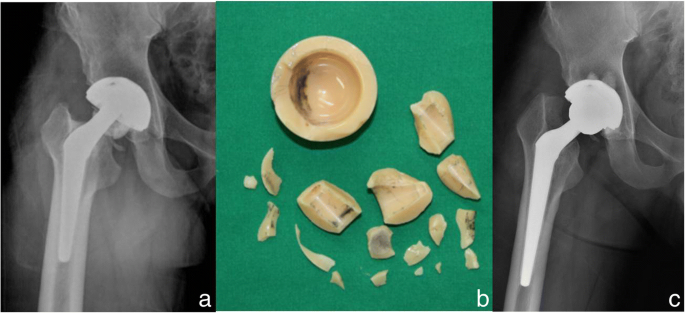
A 34-twelvemonth-erstwhile male patient with right full hip arthroplasty using CoC articulation (Forte) (a) Radiograph with fractured ceramic head and liner (b) The fractured ceramic head and liner (c) Radiographs after revision surgery changing the ceramic liner and fractured caput to metasul liner and metal head after cementing
Another business concern remains squeaking of ceramic bearings. This potentially affects the patient'south quality of lifeand survivorship of the implant due to revision of the squeaky hip. Noises emanating from ceramic bearings (usually clicking and squeaking) take been reported with rates that vary from 0 to 33%. Fortunately clinically the trouble is often modest in themajority of patients and revision surgery is indicated onlyoccasionally. Yoon et al. also reported depression incidence of squeaking (1.5%), and at that place were no complications to limit daily life and no revision [126]. Despite these shortcomings, CoC articulation seems to be the best recently.
Habiliment machinery
The dominating wear mechanism is mild surface fatigue maintaining a polished appearance in nearly areas of the articulating surfaces. The grain structure of the material can exist easily identified in such polished areas. Sometimes, fine scratches originating from the initial polishing process during manufacturing are yet visible indicating a very mild wear process. Abrasive scratches tin exist observed, withal to a much lower extent than in other systems. No tribochemical reaction layers have been reported.
Ceramic on PE (CoP) joint
Advantages
CoP as a begetting couple currently accounts for around one in vii hip replacements in the United kingdom [127]. Potentially this keeps the advantages of the softer, less rigid PE surface and utilises the advantages of the smooth, hard ceramic surface.
Over the period examined, CoP bearing surfaces steadily increased in popularity to go the nigh popular bearing surface blazon. Although concerns near fracturing of the femoral head [128] and increased costs had decreased usage of ceramic heads in the 1980s and 1990s, the appearance of big ceramic heads with depression fracture rates, low wear rates, and multiple cervix length options over the past decade had increased the use of CoP bearings [129].
It is as well credible from the literature that CoC hips accept lower wear rates compared with CoP hips, however, the mid-term studies utilising newer alumina ceramic with newer PEs bear witness no difference in osteolysis or patient satisfaction at v years [130].
Disadvantages
Theoretically, the limitations of CoP bearing surfaces involves the take a chance of alumina head fracture, the resultant hard revision surgery [131], metal transfer which can increase surface roughness, and 3rd body wear leading to increased PE clothing [132]. With the advent of delta ceramic, the rate of fracture decreased dramatically. At that place has been no reports yet, almost the clinically significant trouble coming from metal transfer (Tabular array ane).
Wear mechanism
Information technology may be like to MoP articulation. Vesture mechanism is surface fatigue where the PE part is normally by far more affected than the hard counterbody. Surface fatigue is associated with repetitive loading and generates wear features such as pitting and delamination [133, 134]. The most common wear advent in PE cups is polishing.
Unlike in MoM articulation, no tribochemical reactions have even so been reported for polymer cups. But, this does not preclude their being. PE transfer films on the hard counter parts have been reported [135].
Orthopedic habiliment debris
Article of clothing debris is formed at prosthetic articulation articulations, at modular interfaces, at areas of impingement, and at nonarticulating interfaces due to abrasion with the surrounding bone, or debris [136].
Cells in the periprosthetic surround are exposed to a continuous production of wear particles. The biologic response to particle wear debris circuitous and drives the process toward periprosthetic tissue destruction and implant loosening. Although most of the studies accept focused on UHMWPE particles, particles generated from other sources may induce an inflammatory reaction and subsequent osteolysis [137, 138]. For case, silicate and stainless steel particles, as possible containments from drilling and reaming tools, may elicit an aggressive cellular response. Although they may participate in initiating and/or instigating an inflammatory process, their role is considered minor. Alumina ceramic is a material usually described as bio-inert [139]. However, submicron-sized particulates of alumina and zirconia may arm-twist a like but less intense reaction to those seen with submicron-sized polymers and metallic droppings.
Conclusion
THA remains a highly successful procedure providing good pain relief and improvement of activeness levels. Despiteits success, the expectations continue to increment with more and more young patients undergoing hip replacement and about of them seeking higher activity level (higher range ofmotion and stability in those ranges) as well as longevity of the prosthesis. Too, the fixation method for the prosthesis, good surgical arroyo, begetting surfaces remain the most important determinant of longevity of the hip prosthesis.
Newer bearing surfaces incurrent clinical exercise have shown promising clinical outcomes. With success of these wear reducing bearing surfaces, the scientific community will need to focus on not only farther reducing abrasive wear but on reducing stress shielding too by newer materials likewise as designs. Ongoing research and the futurity of biomaterials in the hip are anticipated.
Abbreviations
- CoC:
-
ceramic on ceramic
- Co-Cr:
-
cobalt-chromium
- CoP:
-
ceramic on polyethylene
- DLC:
-
diamond-like carbon
- MoM:
-
metal on metal
- MoP:
-
metal on polyethylene
- PE:
-
polyethylene
- PMPC:
-
poly (2-methacryloyloxyethyl phosphorylcholine)
- THA:
-
total hip arthroplasty
- TiN:
-
titanium nitride
- UHMWPE:
-
ultra high molecular weight polyethylene
- UND:
-
ultra nanocrystalline diamond
- XLPE:
-
high crosslinked UHMWPE
- ZTA:
-
zirconia-toughened alumina
References
-
National Joint Registry for England. Wales, Northern Ireland and the Isle of man. 13th AnnualReport.http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/13th%20Annual%20Report/07950%20NJR%20Annual%20Report%202016%20ONLINE%20REPORT.pdf. Accessed 2016.
-
Maradit Kremers H, Larson DR, Crowson CS, et al. Prevalence of TotalHip and knee replacement in the United States. J Bone Articulation Surg Am. 2015;97:1386–97. https://doi.org/10.2106/JBJS.N.01141.
-
Kurtz South, Ong K, Lau E, Mowat F, Halpern Grand. Projections of primary and revision hip and kneearthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5.
-
Health Insurance Review & Assessment Service, Korea Healthcare Bigdata Hub. http://opendata.hira.or.kr/op/opc/olapDiagBhvInfo.do. Accessed 14 Sept 2018.
-
Miura K, Yamada N, Hanada S, Jung TK, Itoi Eastward. The bone tissue compatibility of a new Ti-Nb-Sn alloywith a low Young'southward modulus. Acta Biomater. 2011;7:2320–6.
-
Guo Due south, Bao ZZ, Meng QK, Hu L, Zhao XQ. A novel metastable Ti-25Nb-2Mo-4Sn alloy with high strength and low Young'due south modulus. Metall Mater Trans A Phys Metall Mater Sci. 2012;43:3447–51.
-
Niinomi Grand, Hattori T, Morikawa G, Kasuga T, Suzuki A, Fukui H, Niwa S. Development of lowrigidity beta-blazon titanium blend for biomedical applications. Mater Trans. 2002;43:2970–7.
-
Okazaki Y. A new Ti-15Zr-4Nb-4Ta alloy for medical applications. Curr Opin Solid State Mater Sci. 2001;v:45–53.
-
Bai 10, Sandukas South, Appleford MR, Ong JL, Rabiei A. Deposition and investigation of functionallygraded calcium phosphate coatings on titanium. Acta Biomater. 2009;v:3563–72.
-
Bai X, Sandukas S, Appleford MR, Ong JL, Rabiei A. Antibacterial result and cytotoxicity of Ag-doped functionally graded hydroxyapatite coatings. J Biomed Mater Res Part B Appl Biomaterials. 2012;100:553–61.
-
Chen W, Liu Y, Courtney HS, Bettenga K, Agrawal CM, Bumgardner JD, Ong JL. In vitro anti-bacterial and biological properties of magnetron co-sputtered silver-containing hydroxyapatite coating. Biomaterials. 2006;27:5512–7.
-
Ong JL, Lucas LC, Lacefield WR, Rigney ED. Structure solubility and bond force of thin calcium-phosphate coatings produced by ion-beam sputter deposition. Biomaterials. 1992;13:249–54.
-
Yang YZ, Kim KH, Ong JL. Review on calcium phosphate coatings produced using a sputtering process—an alternative to plasma spraying. Biomaterials. 2005;26:327–37.
-
Kim HM, Miyaji F, Kokubo T, Nakamura T. Preparation of bioactive Ti and its alloys via simple chemical surface treatment. J Biomed Mater Res. 1996;32:409–17.
-
Kim HM, Miyaji F, Kokubo T, Nishiguchi S, Nakamura T. Graded surface construction of bioactive titanium prepared past chemical treatment. J Biomed Mater Res. 1999;45:100–7.
-
Kim HM, Takadama H, Miyaji F, Kokubo T, Nishiguchi S, Nakamura T. Germination of bioactivefunctionally graded construction on Ti-6Al-4V alloy by chemical surface treatment. J Mater Sci Mater Med. 2000;11:555–9.
-
Kizuki T, Takadama H, Matsushita T, Nakamura T, Kokubo T. Grooming of bioactive Ti metal surface enriched with calcium ions by chemical treatment. Acta Biomater. 2010;6:2836–42.
-
Kokubo T, Pattanayak DK, Yamaguchi Southward, Takadama H, Matsushita T, Kawai T, Takemoto Thousand, Fujibayashi Due south, Nakamura T. Positively charged bioactive Ti metal prepared by simple chemical and heat treatments. J R Soc Interface. 2010;7:503–13.
-
Oral East, Christensen SD, Malhi As, Wannomae KK, Muratoglu OK. Vesture resistance and mechanical properties of highly cross-linked, ultrahigh-molecular weight polyethylene doped with vitamin E. J Arthroplast. 2006;21:580–91.
-
Oral E, Muratoglu OK. Vitamin Due east diffused, highly crosslinked UHMWPE: a review. Int Orthop. 2011;35:215–23.
-
Kyomoto Thou, Moro T, Konno T, Takadama H, Yamawaki N, Kawaguchi H, Takatori Y, Nakamura M, Ishihara K. Enhanced habiliment resistance of modified cross-linked polyethylene by grafting with poly(two-methacryloyloxyethyl phosphorylcholine). J Biomed Mater Res Part A. 2007;82(1):10–7.
-
Kyomoto 1000, Moro T, Iwasaki Y, Miyaji F, Kawaguchi H, Takatori Y, Nakamura K, Ishihara K. Superlubricious surface mimicking articular cartilage past grafting poly(2-methacryloyloxyethyl phosphorylcholine) on orthopaedic metal bearings. J Biomed Mater Res Role A. 2009;91:730–41.
-
Clarke IC, Manaka M, Green DD, Williams P, Pezzotti Grand, Kim YH, Ries Thou, Sugano N, Sedel L, Delauney C, et al. Current status of zirconia used in total hip implants. J Bone Joint Surg Am. 2003;85:73–84.
-
Begand S, Oberbach T, Glien West. Investigations of the mechanical properties of an alumina toughened zirconia ceramic for an application in joint prostheses. Key Eng Mater. 2005;284:1019–22.
-
Al-Hajjar Yard, Jennings LM, Begand S, Oberbach T, Delfosse D, Fisher J. Vesture of novel ceramic-on-ceramic bearings under adverse and clinically relevant hip simulator weather condition. J Biomed Mater Res Part B Appl Biomater. 2013;101:1456–62.
-
Hobbs LW, Rosen VB, Mangin SP, Treska Thou, Hunter G. Oxidation microstructures and interfaces in the oxidized zirconium knee. Int J Appl Ceram Technol. 2005;2:221–46.
-
Good 5, Ries Thou, Barrack RL, Widding Thousand, Hunter M, Heuer D. Reduced clothing with oxidized zirconium femoral heads. J Bone Joint Surg Am. 2003;85:105–ten.
-
Burger W, Richter HG. High forcefulness and toughness alumina matrix composites past transformationtoughening and 'in situ' platelet reinforcement (ZPTA)—the new generation of bioceramics. Key Eng Mater. 2000;192–5:545–viii.
-
McKee GK, Watson-Farrar J. Replacement of arthritic hips by the McKee-Farrar prosthesis. J Bone Joint Surg Br. 1966;48(2):245–59.
-
Triclot P. Metal-on-metal: history, land of the art. Int Orthop. 2011;35(ii):201-half dozen.
-
Learmonth ID, Young C, Rorabeck C. The operation of the century: full hip replacement. Lancet. 2007;370:1508–19. https://doi.org/x.1016/S0140%2D6736(07)60457%2D7.
-
Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of 2 chiliad consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Os Joint Surg Am. 2002;84–A:171–7.
-
Boutin P. Full arthroplasty of the hip by fritted alumina prosthesis. Experimental report and 1st clinical applications. Orthop Traumatol Surg Res. 2014;100:15–21.
-
Howmedica I. Strength for Life : The Vitallium Alloy Story. Rutherord: Howmedica Inc.; 1995.
-
Bronzino JD. The Biomedical Engineering Handbook. 2nd ed: CRC Press; 1999.
-
Caput WC, Bauk DJ, Emerson RH. Titanium every bit the material of choice for cementless femoral components in total hip arthroplasty. Clin Orthop Relat Res. 1995;311:85–90.
-
Branemark PI, George AZ, Tomas A. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence; 1985. p. 1–76.
-
Landor I, Vavrik P, Sosna A, Jahoda D, Hahn H, Daniel M. Hydroxyapatite porous blanket and the osteointegration of the total hip replacement. Arch Orthop Trauma Surg. 2007;127(2):81–9.
-
Balla VK, Bodhak Due south, Bose Southward, Bandyopadhyay A. Porous tantalum structures for bone implants: fabrication, mechanical and in vitrobiological backdrop. Acta Biomater. 2010;6(8):3349–59.
-
Matassi F, Botti A, Sirleo Fifty, Carulli C, Innocenti Grand. Porous metal for orthopedics implants. Clin Cases Miner Bone Metab. 2013;x(2):111–five.
-
Charnley J. Arthroplasty of the hip: a new operation. Lancet. 1961;1:1129–32.
-
Hopper RH Jr, Young AM, Orishimo KF, Engh CA Jr. Effect of terminal sterilization with gas plasma or gammaradiation on vesture of polyethylene liners. J Os Joint Surg Am 2003;85:464–468.
-
McKellop H, Shen FW, Lu B, Campbell P, Salovey R. Upshot of sterilization method and other modifications on the wearresistance of acetabular cups fabricated of ultra-high molecular weightpolyethylene. A hip-simulator report. J Bone Articulation Surg Am. 2000;82:1708–25.
-
Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titaniumprosthesis. Factors influencing generation of polyethylene debris. J Arthroplasty. 1997;12:256–66.
-
Immature AM, Sychterz CJ, Hopper RH Jr, Engh CA. Effectof acetabular modularity on polyethylene wear and osteolysis intotal hip arthroplasty. J Bone Articulation Surg Am 2002; 84:58–63.
-
Harris WH. The trouble is osteolysis. Clin Orthop Relat Res. 1995;311:46–53.
-
Kim YH, Kim JS, Park JW, Joo JH. Periacetabular osteolysis is the problem in contemporary total hip arthroplasty in young patients. J Arthroplast. 2012;27:74–81.
-
Digas Thousand, Kärrholm J, Thanner J, Malchau H, Herberts P. Highly cantankerous-linked polyethylene in total hip arthroplasty: randomizedevaluation of penetration rate in cemented and uncementedsockets using radiostereometric analysis. Clin Orthop Relat Res. 2004;429:6–16.
-
Manning DW, Chiang PP, Martell JM, et al. In vivo comparative wear written report of traditional and highly cross-linked polyethylene in total hip arthroplasty. J Arthroplast. 2005;20(7):880–half-dozen.
-
Martell JM, Verner JJ, Incavo SJ. Clinical performance of a highly cantankerous-linked polyethylene at two years in full hip arthroplasty: a randomized prospective trial. J Arthroplast. 2003;eighteen(seven suppl 1):55–9.
-
Collier JP, Currier BH, Kennedy Fe, et al. Comparison of cross-linked polyethylene materials for orthopaedic applications. Clin Orthop Relat Res. 2003;414:289–304.
-
Muratoglu OK, Bragdon CR, O'Connor Exercise, et al. Unified wearable model for highly cross-linked ultra-high molecular weight polyethylenes (UHMWPE). Biomaterials. 1999;20(16):1463–70.
-
Chiesa R, Tanzi MC, Alfonsi South, et al. Enhanced wear performance of highly crosslinked UHMWPE for artificial joints. J Biomed Mater Res. 2000;50(3):381–7.
-
Muratoglu OK, Greenbaum ES, Bragdon CR, et al. Surface assay of early on retrieved acetabular polyethylene liners: A comparison of conventional and highly crosslinked polyethylene. J Arthroplasty. 2004;nineteen(i):68–77.
-
Dumbleton JH, D'Antonio JA, Manley MT, Capello WN, Wang A. The basis for a second-generation highly cross-linked UHMWPE. Clin Orthop Relat Res. 2006;453:265–71.
-
Ishihara K. Highly lubricated polymer interfaces for advanced bogus hip joints through biomimetic design. Polym J. 2015;47:585–97.
-
Hannouche D, Hamadouche Grand, Nizard R, et al. Ceramics in total hip replacement. Clin Orthop Relat Res. 2005;430:62–71.
-
Clarke IC, Expert V, Williams P, Schroeder D, Anissian L, Stark A, Oonishi H, Schuldies J, Gustafson G. Ultra-low wear rates for rigid-on-rigid bearings in total hip replacements. Proc Inst Mech Eng H. 2000;214:331–47.
-
Jeffers JR, Walter WL. Ceramic-on-ceramic bearings in hip arthroplasty: land of the art and the time to come. J Bone Articulation Surg Br. 2012;94(six):735–45.
-
Kurtz SM. UHMWPE Biomaterials Handbook. 2nd ed. Boston, mass: Bookish Press; 2009.
-
Masonis JL, Bourne RB, Ries MD, et al. Zirconia femoral caput fractures: A clinical and retrieval analysis. J Arthroplasty. 2004;xix(7):898–905.
-
De Aza AH, Chevalier J, Fantozzi Yard, et al. Crack growth resistance of alumina, zirconia and zirconia toughened alumina ceramics for articulation prostheses. Biomaterials. 2002;23(3):937–45.
-
Allain J, Le Mouel S, Goutallier D, et al. Poor eight-yr survival of cemented zirconia-polyethylene total hip replacements. J bone Joint Surg Br. 1999;81(5):835–42.
-
Masonis JL, Bourne RB, Ries Medico, McCalden RW, Salehi A, Kelman DC. Zirconia femoral head fractures: a clinical and retrieval analysis. J Arthroplast. 2004;xix:898–905.
-
Santos EM, Vohra S, Catledge SA, McClenny Dr., Lemons J, Moore KD. Test of surface and material properties of explantedzirconia femoral heads. J Arthroplast. 2004;19(7Suppl ii):thirty–4.
-
Chevalier J. What future for zirconia as a biomechanical? Biomaterials. 2006;27(4):535–43.
-
Bal BS, Rahaman MN. Orthopedic applications of silicon nitride ceramics. Acta Biomater. 2012;viii:2889–98.
-
McEntire BJ, Bal BS, Rahaman MN, Chevalier J, Pezzotti Chiliad. Ceramics and ceramic coatings in orthopaedics. J Eur Ceram Soc. 2015;35:4327–69.
-
Chen FC, Ardell AJ. Fracture toughness of ceramics and semi-brittle alloys using a miniaturized disk-bend test. Mater Res Innov. 2000;iii:250–62.
-
Bal BS, et al. Fabrication and testing of silicon nitride bearingsin total hip arthroplasty. J Arthroplast. 2009;24(i):110–6.
-
McEntire BJ, Lakshminarayanan R, Ray DA, Clarke IC, Puppulin L, Pezzotti Thousand. Silicon nitride bearings for total joint arthroplasty. Lubricants. 2016;iv:35.
-
Tribe H, Malek Southward, Stammers J, et al. Advanced habiliment of an Oxinium™ femoral caput implant post-obit polyethylene liner dislocation. Ann R Coll Surg Engl. 2013;95(8):133–5.
-
Hernigou P, Mathieu Thousand, Poingnard A, et al. Oxinium, a new culling femoral begetting surface pick for hip replacement. Eur J Orthop Surg Traumatol. 2007;17(three):243–6.
-
Kop AM, Whitewood C, Johnston DJ. Damage of Oxinium femoral heads subsequent to hip arthroplasty dislocation: Three retrieval case studies. J Arthroplasty. 2007;22(five):775–ix.
-
Lewis PM, Moore CA, Olsen M, Schemitsch E, Waddell JP. Comparison of mid-term clinical outcomes post-obit primarytotal hip arthroplasty with Oxinium versus cobalt chromefemoral heads. Orthopedics. 2008;31(12Supppl2).
-
Abu-Amer Y, Darwech I, Clohisy JC. Aseptic loosening of total articulation replacements: mechanisms underlying osteolysis and potential therapies. Arthritis Res Ther. 2007;9:S6.
-
Narayan RJ. Nanostructured diamondlike carbon thin films for medical applications. Mater Sci Eng C. 2005;25:405–16.
-
Pappas MJ, Makris M, Buechel FF. Titanium nitride ceramic film confronting polyethylene: A 48-meg bicycle wear exam. Clin Orthop Relat Res. 1995;317:64–seventy.
-
Hauert R, Falub CV, Thorwarth M, Thorwarth K, Affolter C, Stiefel Thousand, Podleska LE, Taeger G. Retrospective lifetime estimation of failed and explanted diamond-like carbon coated hip articulation assurance. Acta Biomater. 2012;8:3170–6.
-
Catledge SA, Vohra YK. Issue of nitrogen addition on the microstructure and mechanical properties of diamond films grown using loftier-methane concentrations. J Appl Phys. 1999;86:698–700.
-
Catledge SA, Vaid R, Diggins P, Weimer JJ, Koopman M, Vohra YK. Improved adhesion of ultra-hard carbon films on cobalt-chromium orthopaedic implant alloy. J Mater Sci Mater Med. 2011;22:307–16.
-
Papo MJ, Catledge SA, Vohra YK. Mechanical wear behavior of nanocrystalline and multilayer diamond coatings on temporomandibular joint implants. J Mater Sci Mater Med. 2004;15:773–7.
-
Vila Grand, Amaral 1000, Oliveira FJ, Silva RF, Fernandes AJS, Soares MR. Residual stress minimum in nanocrystalline diamond films. Appl Phys Lett. 2006;89:093109.
-
Kumar N, Arora GN, Datta B. Begetting surfaces in hip replacement-evolution and likely future. Med J Armed Forces Republic of india. 2014;70(iv):371–6.
-
Charnley J, Kamangar A, Longfield MD. The optimum size of prosthetic heads in relation to wear of plastic sockets in total replacement of hip. Med Biol Eng. 1969;vii:31–ix.
-
Tsukamoto Chiliad, Mori T, Ohnishi H, Uchida S, Sakai A. Highly cross-linked polyethylene reduces Osteolysis incidence and Habiliment-related reoperation rate in Cementless Full hip arthroplasty compared with conventional polyethylene at a hateful 12-year follow-up. J Arthroplast. 2017;32(12):3771–six. https://doi.org/10.1016/j.arth.2017.06.047.
-
Vendittoli PA, Riviere C, Lavigne Chiliad, Lavoie P, Alghamdi A, Duval N. Aluminaon alumina versus metal on conventional polyethylene: a randomizedclinical trial with nine to xv years follow-upwards. Acta Orthop Belg. 2013;79:181–90.
-
Green TR, Fisher J, Rock M, Wroblewski BM, Ingham E. Polyethylene particles of a 'critical size' are necessary for theinduction of cytokines past macrophages in vitro. Biomaterials. 1998;19:2297–302.
-
Dumbleton JH, Manley MT, Edidin AA. A literature review ofthe clan between wear rate and osteolysis in total hiparthroplasty. J Arthroplast. 2002;17:649–61.
-
D'Antonio JA, Capello WN, Naughton G. Ceramic bearings for full hiparthroplasty take high survivorship at 10 years. Clin Orthop Relat Res. 2012;470:373–81.
-
Brach del Prever EM, Bistolfi A, Bracco P, Costa Fifty. UHMWPE for arthroplasty: by or future? J Orthop Traumatol. 2009;x:1–8.
-
Oral Eastward, Christensen SD, Malhi Every bit, Wannomae KK. MuratogluOK. Wear resistance and mechanical properties of highlycross-linked, ultrahigh-molecular weight polyethylene dopedwith vitamin East. J Arthroplast. 2006;21:580–91.
-
Bragdon CR, Doerner Chiliad, Martell J, Jarrett B, Palm H, Malchau H. The 2012 John Charnley award: clinical multicenter studies of the wear performance of highly crosslinked remelted polyethylene in THA. Clin Orthop Relat Res. 2013;471:393–402.
-
McKellop HA, Campbell P, Park SH, Schmalzried TP, Grigoris P, Amstutz HC, Sarmiento A. The origin of submicron polyethylene wear droppings in total hip arthroplasty. Clin Orthop Relat Res. 1995;311:3–20.
-
McMinn D, Daniel J. History and modern concepts in surface replacement. Proc lnst Mech EngH. 2006;220:239–51.
-
Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip inpatients nether the age of 55 years with osteoarthritis. J Os Articulation Surg Br. 2004;86:177–84.
-
Mauricio South, Christian H, Thomas P. Metal-on-Metal Total Hip Replacement. Clin Orthop Relate Res. 2005;430:53–61.
-
Moon JK, Kim Y, Hwang KT, Yang JH, Oh YH, Kim YH. Long-term outcomes after metal-on-metallic Total hip arthroplasty with a 28-mm head: a 17- to 23-year follow-upwards study of a previous report. J Arthroplast. 2018. https://doi.org/ten.1016/j.arth.2018.02.089.
-
Hur CI, Yoon TR, Cho SG, Song EK, Seon JK. Serum ion level later on metallic-on-metal THA in patients with renal failure. Clin Orthop Relat Res. 2008;466(3):696–9. https://doi.org/ten.1007/s11999-007-0093-iii.
-
National Joint Registry for England. Wales, Northern Ireland and the Isle of Man. fifth Annual Report. http://world wide web.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/5th%20Annual.pdf. Accessed 2008.
-
Australian Orthopaedic Association National Joint Replacement Registry Annual Written report. https://aoanjrr.sahmri.com/documents/10180/42662/Annual%20Report%202008?version=1.1&t=1349406277970. Asscessed 2008.
-
Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metallic bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphologicalstudy. J Os Joint Surg Am. 2005;87:28–36.
-
Jacobs JJ, Hallab NJ. Loosening and osteolysis associated with metal-on-metalbearings: a local result of metallic hypersensitivity? J Os Joint Surg Am. 2006;88:1171–2.
-
Brodner W, Bitzan P, Meisinger V, Kaider A, Gottsauner-Wolf F, Kotz R. Elevated serum cobalt with metallic-on-metal articulating surfaces. J Bone Joint Surg Br. 1997;79(two):316–21.
-
Urban RM, Jacobs JJ, Tomlinson MJ, Gavrilovic J, Blackness J, Peoc'h Yard. Dissemination of vesture particles to the liver, spleen, and abdominal lymph nodes of patients with hip or human knee replacement. J Bone Joint Surg Am. 2000;82:457–76.
-
Case CP. Chromosomal changes after surgery for joint replacement. J Bone Joint Surg Br. 2001;83(viii):1093–5.
-
Smith AJ, Dieppe P, Porter Grand, Blom AW. National Joint Registry of England and Wales Risk of cancer in first seven years later on metal-on-metal hip replacement compared with other bearings and general population: linkage report between the National Articulation Registry of England and Wales and hospital episode statistics. BMJ. 2012;344:e2383.
-
Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis later on contemporarymetal-on-metal total hip arthroplasty. 5 to 9-year follow-upwards. J BoneJoint Surg Am. 2006;88:1183–91.
-
Milosev I, Trebse R, Kovac S, Cor A, Pisot V. Survivorship and retrieval analysisof Sikomet metallic-on-metallic total hip replacements at a mean of seven years. J Bone Joint Surg Am. 2006;88:1173–82. https://doi.org/10.2106/JBJS.E.00604.
-
Park YS, Moon YW, Lim SJ, Yang JM, Ahn G, Choi YL. Early osteolysisfollowing second-generation metal-on-metal hip replacement. J Bone Articulation Surg Am. 2005;87:1515–21. https://doi.org/10.2106/JBJS.D.02641.
-
Administration FAD. List of Device Recalls. … fda. gov/medicaldevices/prophylactic/ListofRecalls/default …; 2014; https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfRES/res.cfm?start_search=1&event_id=&productdescriptiontxt=hip%20arthroplasty&productcode=&IVDProducts=&rootCauseText=&recallstatus=%A2erclassificationtypetext=&recallnumber=&postdatefrom=&postdateto=&productshortreasontxt=&knumber=&PAGENUM=500. Accessed 06 Feb 2018.
-
Boutin P. Total arthroplasty of the hip past fritted aluminum prosthesis. Experimental study and 1st clinical applications. Rev Chir Orthop Reparatrice Appar Mot. 1972;58:229–46.
-
Jonathan PG. Ceramic hip replacement history. Semin Arthroplast. 2011;22(iv):214–7.
-
Kurtz SM, Ong K. Contemporary total hip arthroplasty: Difficult-on hard bearings and highly crosslinked UHMWPE. In: Kurtz SM, editor. UHMWPE Biomaterials Handbook. second ed. Burlington: Bookish(Elsevier); 2009. p. 55–79.
-
Williams South, Schepers A, Isaac G, Hardaker C, Ingham E, van der Jagt D, Breckon A, Fisher J. The 2007 Otto Aufranc award. Ceramic-on-metalhip arthroplasties: a comparative in vitro and in vivo report. Clin Orthop Relat Res. 2007;465:23–32.
-
Park KS, Seon JK, Yoon TR. The survival assay in third-generation ceramic-on-ceramic Full hip arthroplasty. J Arthroplast. 2015;30(11):1976–80. https://doi.org/ten.1016/j.arth.2015.05.017.
-
Lewis PM, Al-Belooshi A, Olsen M, Schemitch EH, Waddell JP. Prospective randomized trial comparing alumina ceramic-on-ceramic with ceramic-on-conventional polyethylene bearings in total hip arthroplasty. J Arthroplasty. 2010;25(3):392–7.
-
Kubo T, Sawada M, Hirakawa M, Shimizu C, Takamatsu T, Hirasawa Y. Histiocyte reaction in rabbit femurs to UHMWPE, metal, and ceramicparticles in different sizes. J Biomed Mater Res. 1999;45(4):363–9.
-
Hernigou P, Zilber S, Filippini P, Poignard A. Ceramic-ceramic begetting decreases osteolysis: a 20-twelvemonth study versus ceramic-polyethylene on the contralateral hip. Clin Orthop Relat Res. 2009;467:2274–80.
-
Si HB, Zeng Y, Cao F, Pei FX, Shen B. Is a ceramic-on-ceramic bearing really superiorto ceramic-on-polyethylene for primary total hiparthroplasty? A systematic review and meta-analysisof randomised controlled trials. Hip Int. 2015;25(3):191–8. https://doi.org/10.5301/hipint.5000223.
-
Glaser D, Komistek RD, Cates HE, Mahfouz MR. Clicking and squeaking:in vivo correlation of sound and separation for different bearingsurfaces. J Bone Joint Surg Am. 2008;90(Suppl(4):112–20.
-
Yang CC, Kim RH, Dennis DA. The squeaking hip: a cause for concern-disagrees. Orthopedics. 2007;30:739.
-
Ranawat AS, Ranawat CS. The squeaking hip: a crusade for concern-agrees. Orthopedics. 2007;30:738.
-
Lusty PJ, Tai CC, Stitch-Hoy RP, Walter WL, Walter WK, Zicat BA. Third-generation alumina-on-alumina ceramic bearings incementless total hip arthroplasty. J Bone Joint Surg Am. 2007;89:2676–83.
-
Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010;468:358–66.
-
Haq RU, Park KS, Seon JK, Yoon TR. Squeaking after third-generation ceramic-on-ceramic total hip arthroplasty. J Arthroplast. 2012;27(vi):909–15. https://doi.org/10.1016/j.arth.2011.ten.001.
-
Lancaster JG, Dowson D, Isaac GH, Fisher J. The vesture of ultra-high molecular weight polyethylene sliding on metallic and ceramic counterfaces representative of current femoral surfaces in joint replacement. Proc Inst Mech Eng H. 1997;211(i):17–24.
-
Callaway GH, Flynn W, Ranawat CS, Sculco TP. Fracture of the femoral headafter ceramic-on-polyethylene total hip arthroplasty. J Arthroplast. 1995;10:855–ix.
-
Lehil MS, Bozic KJ. Trends in total hip arthroplasty implant utilization in theUnited states. J Arthroplast. 2014;29:1915–eight. https://doi.org/10.1016/j.arth.2014.05.017.
-
Rieger W. Ceramics in orthopaedics - thirty years of development and experience. In: Reiker CB, Oberholzer S, Wyss U, editors. World tribology forum in arthroplasty. Berne: Hans Huber Verlag; 2001.
-
Heisel C, Silva Yard, Schmalzried TP. Begetting surface options fortotal hip replacement in young patients. Instr Course Lect. 2004;53:49–65.
-
Della Valle AG, Doty S, Gradl G, Labissiere A, Nestor BJ. Wear ofa highly cross-linked polyethylene liner associated with metallicdeposition on a ceramic femoral head. J Arthroplast. 2004;nineteen(4):532–6.
-
Magnissalis EA, Eliades G, Eliades T. Multitechnique characterization of articular surfaces of retrieved ultrahigh molecular weight polyethylene acetabular socket. J Biomed Mater Res. 1999;48(3):365–73.
-
Collier JP, Bargmann LS, Currier BH, Mayor MB, Currier JH, Bargmann BC. An analysis of hylamer and polyethylene bearings from retrieved acetabular components. Orthopedics. 1998;21(8):865–71.
-
Crockett R, Roba M, Naka M, Gasser B, Delfosse D, Frauchiger V, Spencer ND. Friction, lubrication, and polymer transfer between UHMWPE and CoCrMo hip-implant materials: a fluorescence microscopy report. J Biomed Mater Res A. 2009;89(4):1011–8.
-
McKellop HA. The lexicon of polyethylene wear in artificial joints. Biomaterials. 2007;28(34):5049–57.
-
Berger RA, Jacobs JJ, Quigley LR, Rosenberg AG, Galante JO. Primary cementless acetabular reconstruction in patients younger than 50 years one-time. vii- to eleven-year results. Clin Orthop Relat Res. 1997;344:216-226.
-
Devane PA, Bourne RB, Rorabeck CH, MacDonald S, Robinson EJ. Measurement of polyethylene wear in metal-backed acetabular cups. Ii Clinical application. Clin Orthop Relat Res. 1995;319:317–26.
-
Brawny PJ, Tai CC, Sew-Hoy RP, Walter WL, Walter WK, Zicat BA. Third-generation alumina-on-alumina ceramic bearings in cementless total hip arthroplasty. J Bone Articulation Surg Am. 2007;89:2676–83.
Author information
Affiliations
Contributions
Both authors read and canonical the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Non applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they accept no competing interests.
Publisher'due south Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open up Admission This article is distributed nether the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/past/4.0/), which permits unrestricted apply, distribution, and reproduction in any medium, provided you give advisable credit to the original author(southward) and the source, provide a link to the Creative Commons license, and signal if changes were fabricated. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/null/i.0/) applies to the data made available in this article, unless otherwise stated.
Reprints and Permissions
Virtually this article
Cite this article
Hu, C.Y., Yoon, TR. Recent updates for biomaterials used in total hip arthroplasty. Biomater Res 22, 33 (2018). https://doi.org/10.1186/s40824-018-0144-8
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/x.1186/s40824-018-0144-8
Keywords
- Hip
- Arthroplasty
- Biomaterials
- Stainless steel
- Cobalt-chromium alloy
- Titanium alloy
- Polyethylene
- Ceramic
wickershaterinew2002.blogspot.com
Source: https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-018-0144-8
0 Response to "What Is the Best Material to Use for Hip Replacement?"
Post a Comment